Heat edema is a condition characterized by swelling due to the accumulation of fluid in the body's tissues, particularly noticeable during hot weather conditions. Unlike other types of edema that may result from heart, kidney, or liver problems, heat edema is primarily caused by the body's response to heat, leading to blood vessel dilation and fluid retention. Understanding its causes, symptoms, and treatment options is crucial for managing this condition effectively, especially in warmer climates or during heatwaves.
How is Heat Edema Different from Other Edemas?
Edema is a broad term that encompasses various conditions characterized by swelling caused by the accumulation of fluid in the body's tissues. While there are several types, including pulmonary edema (which affects the lungs and can lead to breathing difficulties) and peripheral edema (often seen in the legs and arms due to circulatory issues, liver disease, or kidney problems), heat edema has distinct characteristics. It specifically occurs as a direct response to elevated temperatures, leading to vasodilation, or the widening of blood vessels, which, in turn, can cause fluid to leak into the surrounding tissues. Unlike edemas stemming from organ dysfunction, heat edema is generally temporary and resolves with cooling measures and movement, highlighting its unique link to environmental conditions rather than underlying health issues.
What Causes Heat Edema?
Hot Weather and High Temperature
The body naturally responds to hot weather by dilating blood vessels to release heat. This physiological reaction, while essential for cooling, can lead to an increased fluid volume in the limbs, particularly when the heat is intense and prolonged. The dilation reduces the return flow of blood to the heart, encouraging fluid to seep out into the surrounding tissues, leading to swelling.
Sun Exposure
Prolonged sun exposure raises the body's surface temperature, further exacerbating vasodilation and fluid retention. The direct heat from the sun not only accelerates the body's need to cool itself but also increases the risk of dehydration, which can paradoxically lead to increased fluid retention as the body attempts to hold onto water.
Physical Activity in Heat
Exercising or engaging in physical activities in hot conditions magnifies the body's heat production. To manage the increased body temperature, blood flow to the skin increases, heightening the risk of fluid leaking into tissues. This risk is compounded if hydration is not adequately maintained before, during, and after activity.
Chronic Diseases
Individuals with pre-existing chronic conditions, such as heart disease, kidney disorders, or diabetes, may have compromised fluid regulation mechanisms. In hot weather, these conditions can make individuals more susceptible to fluid retention and heat edema, as their bodies may struggle to adapt to the increased demands placed on their circulatory and excretory systems.
Pregnancy
Pregnancy induces significant hormonal changes that can affect blood flow and fluid regulation. The increased body weight and the uterus exerting pressure on pelvic blood vessels exacerbate the tendency for fluid to pool in the lower limbs. Heat adds an additional burden, making pregnant women particularly prone to heat edema.
Prolonged Standing or Sitting in One Position
Remaining in a static position for extended periods can hinder blood circulation, particularly in the lower extremities. In hot environments, this can facilitate fluid accumulation in the feet, ankles, and legs, as the heart pumps blood less efficiently against gravity, leading to edema.
Symptoms of Heat Edema
Swelling and Puffiness
The most immediate sign of heat edema is swelling, typically observed in the feet, ankles, and legs, though hands and arms can also be affected. This swelling is often more pronounced after prolonged periods of sitting or standing and may decrease after a night's rest.
Pain in the Affected Area
While not always painful, the swollen areas can experience discomfort, especially when pressure is applied. The stretching of the skin and the increased fluid pressure against nerves in the affected areas can lead to sensations ranging from mild discomfort to more noticeable pain.
Changes in Skin Texture
The skin overlying the swollen areas may appear stretched, shiny, and feel warm to the touch. This change is due to the increased fluid beneath the skin's surface and the heightened blood flow attempting to cool the body.
Difficulty in Moving the Affected Area
Swelling can restrict the range of motion, making it challenging to move affected limbs normally. This stiffness and discomfort can impede daily activities, although it typically resolves with movement and elevation.
How to Cure Heat Edema?
Elevate the Affected Area
Elevation helps to improve blood circulation and encourages fluid to move away from the swollen areas back toward the heart. Whenever possible, rest with the affected limbs raised above heart level to reduce swelling.
Hydrate
Proper hydration is crucial, especially in hot weather. Drinking adequate amounts of water helps to maintain blood volume and pressure, facilitating the kidneys' ability to excrete excess fluid and reducing the tendency for fluid to accumulate in the tissues.
Avoid High Temperatures
Seeking cooler environments, such as air-conditioned spaces, or taking cool baths or showers can help lower body temperature and constrict blood vessels, mitigating fluid leakage into tissues.
Physical Activity
Light to moderate exercise promotes circulation and aids in pumping fluid back into the bloodstream from the tissues. Activities such as walking or swimming, which involve movement of the limbs without excessive strain, are particularly beneficial.
Limit Salt Intake
Excessive salt in the diet can cause the body to retain fluid. Reducing salt intake can help prevent additional fluid retention, easing the symptoms of heat edema.
Apply Ice Packs
Cold compresses or ice packs applied to swollen areas can provide temporary relief by reducing inflammation and causing blood vessels to constrict, which can help to push fluid away from the affected tissues.
Conclusion
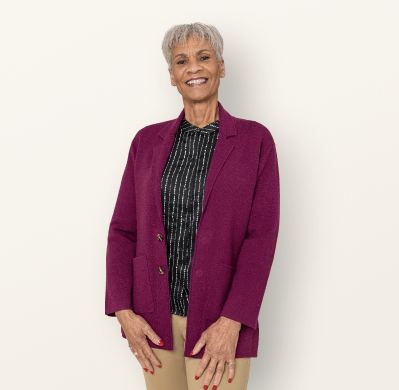
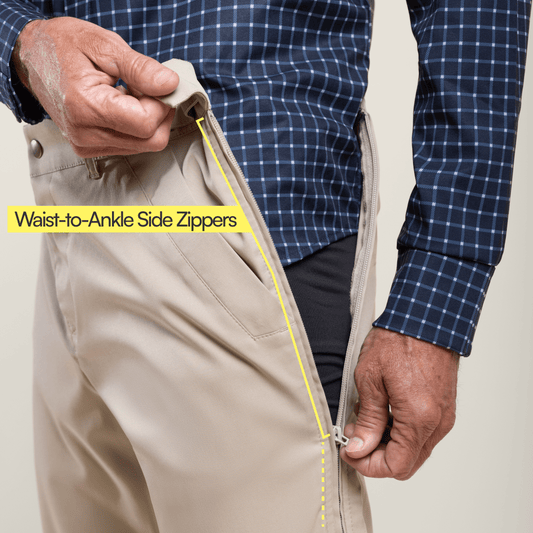
Heat edema, while uncomfortable, is typically a temporary and manageable condition. Recognizing its causes and symptoms allows for timely and effective treatment, primarily focusing on cooling the body and improving circulation. By staying hydrated, avoiding excessive heat, and practicing simple remedies like elevating affected limbs, most individuals can effectively mitigate the effects of heat edema and enjoy a more comfortable experience during hot weather periods. You can also choose to wear comfortable adaptive clothing such as gripper socks that helps with ease in movement.