Tips for Caregivers from the Alzheimer's Association
Hadi Finerty is the Senior Manager of Education & Community Volunteers at Alzheimer's Association Illinois Chapter. In her role, Hadi provides educational programs and individual counseling to caregivers and families who are providing care for those with Alzheimer’s. In the conversation below, Hadi provides advice around many challenges caregivers face when helping their loved ones dress.
We're working with the Alzheimer's Association in the fight to end Alzheimer's. You can donate to The Longest Day charity drive here.
A Personal Caregiving Journey
Ben: Hadi, how did you get involved with the Alzheimer's Association?
Hadi: For me, it was personal. My grandma had Alzheimer's and we were her primary caregivers. I saw that the Alzheimer's Association had an opening and I just applied. And here I am eight years later.
Ben: What do you do at the Alzheimer’s Association?
Hadi:I do education programs for the community. And I think every time I speak to a family, it's just a rewarding experience to be able to help and provide resources. So I think that's what keeps me going, is just the feedback and talking to people and being a part of their journey. There are some people that I've known through the years who have been a part of some of my caregiver classes and we still keep in touch. So it's good to hear how their loved ones are doing on this journey as well.
How Alzheimer's Association Helps Families
Ben: When families reach out and are looking for help, are there some big, common areas they all are looking for or is it more individualized?
Hadi: It can be pretty individualized. But there are some common themes. Often, family members are not all on the same page. Somebody is in denial about the disease or in disagreement regarding the course of care and treatment. Others reach out needing help around specific behaviors like wandering. A lot of people ask for help with basics around daily care.
Why it's hard for people living with dementia and Alzheimer's to get dressed and undressed
Ben: At Joe & Bella, we focus around a certain aspect of daily care. Our founder’s grandfather had Parkinsonian dementia and his grandmother had mobility issues and eventually had some dementia, too. During the pandemic, he put a tablet in her room so the family was able to “drop in” and observe herncare. He observed a caregiver putting a cardigan around her while she was sitting in a wheelchair. And it was the first time everyone really saw it was painful and frustrating the process of getting dressed was for. That was one of the moments that inspired Joe & Bella. Here’s one area where we could hopefully play a meaningful role in making this a little easier for people.
From your perspective, what are some of the most common challenges that people living with dementia and Alzheimer's face when they're getting dressed and undressed?
Hadi: I thought about this a lot because my grandma had the same issue getting dressed as you describe. Sometimes they might not remember exactly how to dress or maybe they're overwhelmed with the choices that they have or the task itself. And of course they might have mobility limitations in addition to their Alzheimer’s or dementia diagnosis.
Four outfits is too many choices for most people with dementia. So it's good to narrow it down. And just like for my grandma, for instance, we just laid out her outfit for her each day and that's what she wore. Some days she needed help because as the disease progressed, she sometimes forgot how to put the sweatshirt over her head.
And when I was looking at your website, I loved that you have adaptive clothing because those clothes make it so much easier to get dressed. Some adults won’t have to worry about buttons in the front, for example. They get fixated on things, and sometimes that's something that can trigger them.
Buttons on the front of the shirt are totally fine. But for some people, they might fidget with them. Maybe they'll pull them off. In the beginning when my grandma was in the early to middle stages, we would put cardigans on her. But we noticed as she was getting toward her middle to late stage, putting those cardigans on got more difficult. And when I talk to families, a lot of them say they have noticed as the disease progresses, sometimes those simple tasks get more difficult. They might want to button the shirt themselves, but struggle using buttons that require fine motor skills.
Alzheimer's and Skin Sensitivity
Ben: Several months ago I spoke to a woman who had early-onset dementia and she was wildly articulate about how the disease affected her on a daily basis. She told me that she wants to wear pajamas all day and she never wants to take them off. And I think some of that had to do with decision making, as you mentioned. Other times she said it just felt like a second skin to her and she felt vulnerable taking it off and felt uncomfortable putting new clean clothes on. I've read that many with dementia and Alzheimer's become very tactile. Have you seen this situation where people's skin gets extra sensitive or they just don't want to change either out of pajamas or into a new outfit?
Hadi: Yeah, and I think you just nailed it. I think it's mostly about decision making. They don't want to think about it. It's like going back to the issue of too many choices. I haven't actually heard anyone really talk about skin sensitivity related to clothing. I know touch is something that's huge for people with the disease. They like to hold hands. Put your arm around them, touch different types of materials, so that makes sense that she might have gotten used to a very specific feeling on her body, and wanting to avoid new sensations.
Aggressive Behavior When Changing Clothes
Ben: We conducted some focus groups a few months ago just to better understand the dressing process for professional caregivers who work in memory care and for family caregivers who provide care at home. And we spoke to one gentleman who was caring for his wife. He was several years older than her. So he always thought that the caregiving in their relationship would have reversed roles. He was far from prepared for this. He didn't know how to iron and hadn't cooked a meal in decades. He said his wife gets aggressive when she changes clothes. She'll hit him and yell at him. And he said that it's like this twice a day, everyday. Do you have any advice for family caregivers who deal with aggressive behavior from their loved ones?
Hadi: I recommend keeping closets free of excess clothing. My grandma’s drawers, of course, had the basic essentials that she needed. But what we noticed is sometimes she would panic if there were too many choices in the closet. Then she would become very overwhelmed. And it was weird because my grandma was Greek, so she didn't really wear a lot of vibrant colors. She liked monotone clothing. But she started gravitating toward purple as her disease progressed. She loved hot pink. And we're like, okay, this is surprising, but we're going to go with it. So we started to fill her closet with those colors, and we just offered two choices. It was either a purple shirt or a pink shirt. We didn't have a ton of variety. And then, of course, in a separate closet, my mom had all of her good clothes, like if we were to go somewhere. I think it's important to organize the process, lay out the clothing in order which item should be put on first.
As the disease progresses, a lot of times they're going to forget how to do this job. We used to hand my grandma one item at a time and we gave simple, direct instructions. "Put your arms in the sleeve." Or "Pull up your pants."
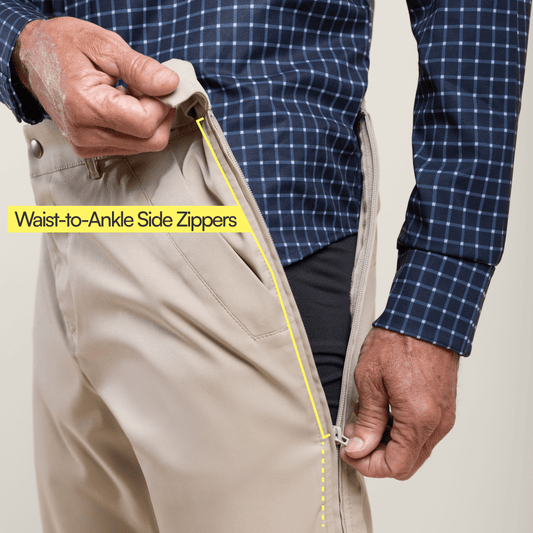
On your website, I love that the pants have magnets. I think that is amazing. You don't have to worry about a zipper fly being down, because that's one more thing they have to worry about. Velcro is something that is awesome to use too. It just depends on the clothing. We have to make sure that the clothing is loose fitting, especially around the waist and their hip area. Because what happens if it's too tight sometimes they can't vocalize that it's too tight. So they might be saying that they're in pain, but they can't explain what hurts or why.
So here's an example. There was a gentleman whose wife told me that for two years he complained about his stomach hurting. They went to the doctor, had ultrasounds. He had bloodwork. They could not figure out why he was complaining about his stomach.
And one day while they were driving in a car, he was fidgeting with his belt and he kept saying that his stomach hurt. Every time he put his belt on, he put it on too tight. The belt buckle was basically stabbing his stomach, but he could not see that. And she said for two years, the doctors were like, “Ma'am, nothing is wrong. Nothing is wrong.”
It's so important to be flexible in your caregiving. We're so used to always wanting our clothes to match. Some people with Alzheimer's could care less what they're wearing as long as it's comfortable. In the beginning, my grandma wore green sweatpants and a purple top. I think we have to just be flexible. If they're happy, then we just need to be happy. It's important to be adaptive. Things are going to change and we just have to be flexible.
Communication Tips
Ben: What are some of the better ways to connect and communicate with your loved one, to understand what their needs are? How can you communicate what your needs are for them? What sort of strategies do you have in terms of communication?
Hadi: One of the things I learned early on when I started working at the Alzheimer's Association, and I wish I knew this on my own caregiver journey, was to meet the disease where it's at. People, especially caregivers, tend to want to argue. And that's not the reality. The reality is for your loved one to define: if they say the grass is blue, the grass is blue. That's the reality. It's really important to not criticize. It's hard, especially when it comes to spouses because it can be frustrating when they don't understand what you're trying to say. We have to meet them where the disease is. I think patience is a virtue, especially when it comes to repetition. As caregivers, we have an array of different roles. You are their activity director, their nurse, housekeeper, and cook. The list goes on. But I think when we communicate, we really have to just make sure to not treat them as kids; we still must show respect for them. For example,sitting next to them where you are eye-to-eye at their same level is much better than standing and towering over them. And a simple touch can really help; if you see that they're getting heated, just gently touch their hand – that's all. That might be all they need to reconnect and refocus. Sometimes saying something like, "I understand what you're saying," and then reassure them and redirect them to something else is an effective way to help them relax and refocus.
Ben: Can you expand on that for a bit? I think it's really helpful to know how to position your body, how to use touch, and how to directly communicate in a respectful way when trying to get a message across.
Hadi: Just being flexible in how you communicate. If they don't like talking at a particular moment, for example, you can change your line of questioning and just go for yes or no questions that are easier to respond to.
You should ask questions one at a time, yes or no, and give them plenty of time to process or respond. Don't rush them. Trying to get them to communicate with you like they used to will just result in both of you getting frustrated.
How to Avoid Caregiver Burnout
Ben: Caring for my grandmother from a distance was a challenge, and that was with a whole team of professionally trained caregivers behind us. And so I just can only imagine living and breathing caregiving 24/7. Caregiving is an overwhelming and challenging experience for so many people, particularly because when most of us become a caregiver, it's not like we’ve had years of training and or even years or months to emotionally prepare for it. Usually we become caregivers around under some sort of urgent or relatively urgent situation, and I know it can be really stressful, frustrating, and challenging. So what do you say to caregivers who are just at their wit's end with their care partner, really trying to be their best caregiver, but are struggling to care for themselves?
Hadi: Patience is a virtue and a skill. If you need to walk out of the room for a minute and take a few deep breaths, by all means do that. Take time for yourself. That's important. A lot of caregivers feel like they have no one else to turn to for help. When your loved one is content, maybe they're doing an activity or watching television, you can take the time for yourself. Maybe it can be a quick shower, or 10 or 15 minutes of mediation or reading or doing something else you like that will relax you. In the beginning stages of the disease, you are able to still go do stuff on your own. Maybe it's a 15-minute walk outside, maybe it's literally just taking yourself outside to read and just being away from the inside of the four walls of your home.
I think it's also important to ask for help. That is huge. Caregivers want help, but often don't necessarily know how (or who) to ask. So I always encourage people to put a list on your refrigerator of things that friends can do to help, and just have it handy when somebody does offer help. While some people might offer an empty gesture, don't let them off the hook! Caregiving needs to be a team game. Your list allows you to not have to even think about it and you can quickly tell them what you need. Even if it's something as small as forgetting to take out your garbage because you have so much going on. Ask your neighbor to take it out for you. Or to hang with your loved one while you go for a 30-minute jog or run to the store.
I moved back home to help my mom take care of my grandmother and my stepdad. He just was her primary caregiver. My grandma forgot all her English at the end, and only spoke Greek. There were two older ladies in the neighborhood who spoke Greek who went to our church. And one day they came up to me and asked if they could come and just sit with my grandma. Could they bake cookies with her? My mom loved it. Of course, in the beginning I felt like I was taking my child to kindergarten even though she was at our house. I kept peeking in because I was nervous. But just them being there for an hour freed up the time for my mom to be able to go take a walk or run to the grocery store. I think asking for help is huge and there are people out there who want to help. They just don't necessarily know how they can help. So have that list ready for when people do ask.
How Adaptive Clothes Helps
Ben: You mentioned when making clothing choices for your grandmother that you were surprised that she liked all these colorful choices, which was new to her. When many older adults move to a care community, they feel some sense of loss of their past life and identity. They moved out of their home. They obviously couldn't bring most of their stuff with them. We set up their room to make it feel as much like home as possible. My grandma’s overflowed with family photos, a couple pieces of her favorite furniture, with stuff hanging on the walls that used to be on the walls of her bedroom. And she wore the same clothes they had always been wearing. And when we tried to get my grandmother to wear adaptive clothing, she refused, even though she was in horrible pain and it was a terrible situation every time she put on our clothes. She refused to wear them because she didn't like how they looked. She thought they were ugly. She would rather put up with all of that pain all of that time because she wanted to look how she wanted to look. And it seemed to me that was just a poor way for her to latch on to her identity or the previous phase of her li`fe. (This struggle of course inspired us to create Joe & Bella clothing that’s both functional and beautiful.) How do you see clothes as playing a role in helping those who have dementia or Alzheimer's retain their identity and express themselves?
Hadi: I think making those clothing choices is important. But I was looking at your website and believe, based on the options you offer, most older adults can still do all that while wearing clothes that properly function for them. I love the pants with magnets instead of buttons. When I get older, I want to wear jeans and a t- shirt. I've worn this my whole life. So finding clothes that I like to wear, but maybe are adapted like those pants with magnetic buttons, is the best of both worlds. Joe & Bella is full of cute, trendy clothes.
And I think a lot of the time, even for the women that I work with, there are so many people who tell me that their mom never wore pants, all she wore was dresses or skirts her whole life. And now she'll never put on a dress or a skirt again. So habits do change for some. Sometimes our identity, or how we want to look, changes over time. Not all older adults want to dress in 2022 like they did in 1982. So I think the easier it is for them to put on their clothing, the more independent they can remain, which is so important. Of course, as the disease progresses, it's going to get harder. They're going to need assistance, and the clothes you offer are a fantastic solution to helping them wear clothes that look great and aren't difficult to put on with some assistance.
Joe & Bella's Adaptive Apparel Collections:
Men's Adaptive Clothing | Women's Adaptive Clothing | Men's Adaptive Shirts | Women’s Adaptive Shirts | Men's Adaptive Pants | Women’s Adaptive Pants | Gripper Socks | Side Zipper Pants | Compression Socks | Best Adaptive Clothing | Adaptive Apparel