By Jennifer Pasternak, Executive Director, Northbrook Inn Memory Care; Advisory Board Member, Joe & Bella
So, you’ve made the decision to move your loved one into memory care. You’ve reviewed our previous blog to help evaluate if it's time for your loved one to move.You’ve spoken with a few memory-care communities and hopefully have toured a couple as well (even if virtually). So, what should you expect when it comes to your family member’s adjustment and acclimation into the memory-care community?
Executive Jennifer Pasternak of the Northbrook Inn advises family members to temper their expectations. Change is almost always difficult, and people need time to adjust. And, during these Covid days, the adjustment is more complicated and challenging.
--------
Anyone moving into a new community in 2020, and at least some of 2021, will need to quarantine in their own room upon arrival for several days; of course, this requirement doesn’t make for an easy transition. Imagine moving into any situation and knowing that you’d be forced to essentially isolate from your peers for 10 days. So, what our leadership team and caregivers do now is to spend as much time as possible with our residents in their rooms. For example, rather than sitting at my desk to catch up on email or other work, I’ll grab my laptop and head to a new resident’s room. Even if they’re not in the mood for talking, having that simple human companionship can mean so much. I’ve gotten used to just hanging with new residents in their rooms while they’ve got the TV on, and at times not saying a whole lot. The last thing we want is for new residents to feel isolated and alone. This is just one of the ways that we try and combat those feelings.
Please also understand that the transition into memory care is different than into assisted care. The latter certainly has its challenges, oftentimes based upon mobility and other physical needs. In memory care, we deal with those same needs, but our residents have additional challenges, based on their changing level of dementia.
What we’ve found is that these Covid times have slowed down an individual’s adjustment to memory care. People behave differently when they need to be quarantined at the beginning of their stay; it delays the natural process of integration. But, everybody’s different. We recently had somebody move in who seemed to really enjoy time alone with his room, watching TV, and receiving visits by our team. He’s like the happiest guy ever, but he was almost too comfortable in his room. So, once his quarantine ended, he didn’t really want to emerge from the comfort and security of his room. It took lots of encouragement to get him out and about. As healthcare professionals, we’re aware of how behavior has changed due to the pandemic and are active in monitoring these shifts, and intervening appropriately to encourage healthy socialization during new residents’ transitions.
Of course, everybody’s different and the nature of their adjustment will be influenced by their stage of dementia.
Still, when families ask me what to expect, I encourage them to be patient and to think in terms of the first 24 hours; the first week; and the first month.
The First 24 Hours
I believe the first 24 hours are more difficult for family members than for residents, especially those with dementia. Because new residents aren’t at all familiar with us, they tend to be on their best behavior. They’re incredibly polite and their “behaviors’ (i.e., those that are driven by their dementia) are often muted.
Everyone comes with a story that was told to them by their family members as to why they’re making the move. These stories are often quite effective in accelerating the resident’s acceptance of what they typically believe is a temporary move. Maybe they recently injured themselves and were told that they’ll receive better care here until they’re ready. One husband actually turned off the heat in his home, explaining to his wife that she needs to move in order to be warmer. These residents never seem to question the “story.” And, the name of our community, the Northbrook Inn, sounds like it’s a hotel. So, residents begin to slowly adjust and assimilate.
Of course, most family members worry about the adjustment and often feel riddled with guilt. They’re of the generation who said, “Never put me in a home.” And their idea about what is a “home” is often based on a perception of “nursing homes” or institutional settings. So even though family members have toured our community and see how different it is from what may be their anachronistic perception of nursing homes, it’s still difficult at times for them to break through that barrier and internalize that places like Northbrook Inn are full of warm, empathetic, caring professionals, who will take wonderful care of their loved one.
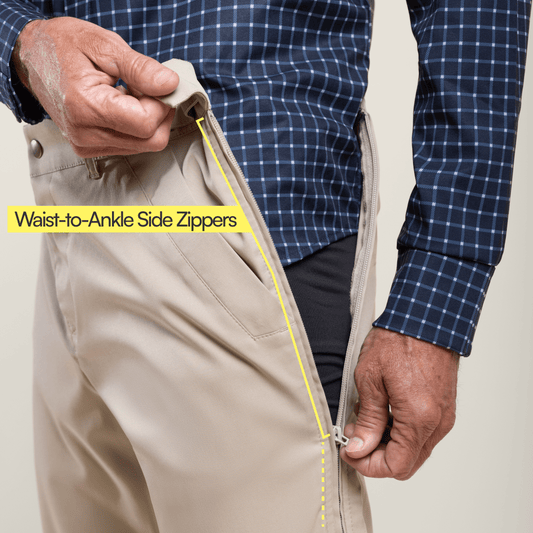
Now, here’s a practical tip: Pack at least a week’s worth of clothes. We don’t allow residents, for example, to wear the same pajamas for more than one night without being washed, which is part of infection control. We also recommend bringing or ordering the same toiletries that you loved one used at home. They know the products’ scents, which can be comforting. In fact, as much as you can, recreate their home in their new room -- if there was a particular photo on your loved one’s nightstand, make sure it gets placed on the nightstand in their new room. While their bed might be a different size, you can decorate it with throw pillows from home, or place a small rug at their feet. Most residents love their rooms when they’re full of family photographs and keepsakes.
The First Week
After the first few days, new residents have started to settle in; and, this is the time when their behaviors typically begin to show. Some residents won’t want to take their meds (and they’re certainly not used to their meds being administered by nurses). We’ve also seen lots of folks who haven’t been showered in weeks (bathing can be a sensory issue -- taking their clothes off, stepping onto a cold floor, feeling water all around them, etc.). When the showering responsibility switches from a family member to a caregiver, showering looks different. Here, we’re trained to always guide the resident to step in front of the caregiver, so we can carefully lead them. We know how to get them to feel more comfortable and to cooperate. They oftentimes sense frustration from their family caregiver at home, which exacerbates their behaviors. We even have one caregiver who will call the “shower whisperer,” due to her ability to calm even the most shower-anxious residents.
Some might not want to eat. The food is different than at home – how, what, and when we serve (and who’s sitting at the table with them). Maybe they’ve been happily living on sandwiches at home; we can do that here in the short-term, to help them transition to our more nutritious (and I’d say delicious) meals.
I think fear of the unknown is why behaviors often lag behind, which seems to make the transition easier than expected. We had a new resident move in a couple of months ago, but it didn’t take her long to start exhibiting behaviors. We understand that every behavior has meaning. Is she hungry? Does she need to go to the bathroom? There’s always a reason. Our job is to find their trigger, to identify what’s ticking them off and then to help work the resident through that trigger to find a solution.
The transition is especially tough now because of Covid. We don’t have the advantage of having family members in our community to help get their loved ones acclimated. Moving in is now literally what we hate to call a “dump and drive.” The family member can’t set up their room or walk them around with them. But, we’re finding creative ways to work around this change and have discovered advantages. In some ways, for family members, the drop-off to our loving team can be an instant relief, and the guilt of not being able to be there is gone.