Over the past year, we’ve been fortunate to speak with a wide range of experts in the caregiving world. From executive directors at care communities, to gerontologists, family caregivers, and even some living with dementia. Many of them provided valuable advice for those beginning their caregiving journey.

Janice Swink, living with early onset dementia:
You can't prepare for it because I don't know what's going to happen. I could lose my balance all of a sudden, without warning. So I'm prepared in a sense, for surprises all the time.
I hope that people try to understand all the different things that happen to people with dementia that are beyond our control.
I want other people with dementia to know that they’re not alone. There are a lot of us out here. I just want to help people. How can I take something so horrible and make something good out of it? When I started out on Twitter a few years ago, I had like two people following me and then I started sharing. And soon a couple thousand people followed me, and that just blows me away.
I used to love to dance. I can't do it much now, but I wanted to show that, even though I had dementia, I could still do something that I loved. It’s frustrating now because I've liked to dance since I was a little girl and no longer can
Anthony Crillo, healthcare and caregiving expert:
There are a lot of important issues to sort out. Is your house equipped for aging in place? Do you have universal design that can accommodate any age or disability? These are questions that you probably don't immediately think of. And what type of care does mom or dad need? Especially if you're pulling them from a skilled-nursing facility or memory care, you're going to need that kind of care at home. And that's one of the things about caregiving: there's an undue burden on family caregivers to take up the role of nurses. And imagine doing that in the middle of a pandemic, when many have lost their jobs, or are now working from home while also running a daycare or school out of their home for their kids.
And then there's the mental and emotional impact, and unresolved family issues that play a role in this decision. If you want mom or dad to come live with you, from a practical standpoint, you need it to physically work with your current living situation. I didn't have a downstairs bedroom when my mom needed more care, so we had to move mom to an independent-living community. So even if this pandemic had hit while I was caregiving (mom passed away in 2016) and we were thinking about pulling her out, I don't know if we could have done it. I don’t think we could have provided enough quality care while balancing everything else going on in our lives.
So it really just puts a big burden on families. Healthcare of the caregiver has always been a huge issue. How many of us have seen our own doctor in the last year? How many of us have not taken the needed self-care or found personal space?
Carol Marak, expert and author, on aging while single:
Make sure you stay social. Make sure you can stay connected. Figure out transportation. Can you drive? If you can't, how else are you getting around? I don't like to drive, but I have easy access to Uber and Lyft. I can walk to the grocery store. How am I going to go shopping if I can't drive one day? Do I have someone checking in on me? Fortunately, we live at a time where technology helps us safely age solo. For example, I also use an app that keeps me checked in with people so they know I’m safe. I even use the free version and it's simple. It sends me a little message: “Are you okay this morning?” I click “yes” and move on with my day.
Lucinda Koza, caregiver to her father:
I never asked for all that responsibility. This has all been sprung on me and disrupted my life. It's unpaid labor, it's so, so much responsibility. It's stressful. It's so many things. Caregivers are part of an invisible unpaid workforce. But if we didn't exist, there would be so much more tragedy in this world. Healthcare systems want positive patient outcomes. They want to decrease hospital re-admittance. And the only way that they can really do that is by communicating with the family caregiver and empowering the family caregiver --- because that's the key to the patient -- not having to go back to the hospital. Family caregivers feel guilt, or a loss of their own independence because we have a lot of power. And it's up to us to take control over our own lives, to find ways in which we can rest, perform self-care, so that we're at our best when our loved ones need help.
Lisa Marie Chirico, wellness coach and caregiving expert:
We all have the ability within us to shift away from the mundaneness of our everyday world and to see ourselves as the magnificent beings that we are, and to see the magnificence in all of us. We're flawed. We're human. We're sick; we're dying. But we have this magnificent light in all of us. So to shift away from despair and fear is not an easy thing. But I do have techniques for my clients to practice. It doesn't happen overnight.
If you're going to see a loved one at a nursing home and are just full of guilt, it's not going to be a good visit for you and your loved one. So you need to shift the focus to something positive for both your sakes
Sheri Snelling, caregiving expert and social gerontologist:
Having a sense of control comes through routines. We can't control disease, like cancer or Covid, and that creates anxiety, stress, and sometimes depression. It’s really hard not to be able to control certain things. Watching a loved one decline and trying to figure out how you can best help is tough. But we can react to these pressures. Create a routine that both you and your loved one can look forward to each day.
You want to make sure you have balance in your life. So you have your own job to do, on top of caregiving responsibilities and caring for yourself. You have to look at all those buckets as equal. If they're not, it’s a natural phenomenon that one of these buckets will suffer if you spend too much time in one of the other buckets. There are plenty of people who sacrifice too much for the sake of their caregiving duties. This results in their getting physically and emotionally burnt out, negatively impacting their caregiving on top of neglecting themselves.
Routine helps – you now have an appointment on the calendar, you can’t accept another meeting, you can’t justify making an excuse to avoid it. And then you’re present and engaged; you’re happy, you're sharing. You made that connection. Just like your morning bathroom routine, you have to make these things a routine to stick. In a 24-hour window, it might not happen every day -- but at least try -- you have to find your “me time.” Carve it out and plan it. Put it on your calendar. Make an appointment with yourself. Even if it’s 10 minutes a day you’ll do X, whatever that is. Listen to a podcast, read a book, take a walk. Whatever makes you happy and gets you to unplug from your daily stressors. It’s hard to do. But you really do have time for 10 minutes for yourself. I know every caregiver can find 10 minutes, as busy as they are. And having that break will payoff for you in the long term. It will help you remain more focused and engaged during your other responsibilities.
Anna Cantor, dementia coach:
There's definitely a process to work through, like a feeling of guilt. It's important to talk through it. How does the guilt make you feel? It's important to create awareness around it, rather than saying it's not good and you should never feel guilty because that just doesn't help in any situation. Because the thing with dementia is that even if you do know sooner, there's nothing that's going to stop it because it's chronic and fatal. The only thing I wish is that I would have been able to spend more time with my mom before she started to change, and that's something that sits with me and I live with.
My best advice is to get a coach. Find someone to talk to. Being a care partner shouldn’t be solely your burden. Whether that is having a meeting with a therapist or going to a support group once a month, that might be all the support new partners need. There are so many different kinds of resources out there; new care partners just need to be proactive and find those resources.
Jackie Melinger, financial advisor for older adults
It is so important to plan and document: Make sure legal documents are in place including your Will, Trust documents, and Power of Attorney for both Property and Healthcare. It is vital that there are trusted professionals involved to help with planning. Most importantly, adult children need to have the courage to talk with their parents well in advance, when they're healthy. Take time to learn about what they want when they get older, what they don't want, what position they're currently in and what position, financially, they think they'll be in a few years from now. It's important for loved ones to know this information. These can be difficult conversations but they are necessary.
Ask them these questions:
- "Mom and dad, what is your financial position for retirement?"
- "Are you going to be able to afford to live life the way you want to in your older age?"
- "Do you have long-term care insurance?"
- "Do you have life insurance?"
- "Do you want to, at all costs, remain at home if you can afford to?”
- “Do you want to move to assisted living or some other type of community where it's more social?"
You don't have to pry for all the details but you should know the general answers to these questions. If they aren't willing to share right then, ask them if they can write the down, so they’re documented. If you can talk about end of life, as hard as that is, you’ll be better able to abide by your loved one’s wishes. I
Betsy Philips, real estate agent for older adults:
Get as much help as you can. Don't be afraid to ask for help. Reach out to a senior real-estate specialist. There are senior coordinators and care coordinators. There are people that manage moves. There are people that want to help you. We all can help you. We can help with every budget. Just please don't be afraid to ask for help. Sooner is always better.
Joy Johnston, family caregiver, advocate and author:
My point in writing my book was hopefully to allow other people to recognize that it's okay if you have a strained relationship with your loved ones that you're caring for -- you can still manage it. And if you feel like you are at the point where you can't manage it, then you need to bring in that outside help.
I think it's really important for people to think about elder-care issues before they face them on a personal level. It's always easier to do so beforehand. I say this, by the way, having not done so myself. There's only so much that you can do ahead of time. It's a very uncomfortable topic for a lot of people, but I really encourage people to sit down with their loved ones and go over the information about end-of-life care. Do they have a will? What are their health-care wishes and end-of-life care wishes? These are really important things.
I would also suggest people think about aging in place. That's what everyone wants to do, right? Or that's what most people want to do. But where are your loved ones living? Are they going to be able to age in place successfully? So start the research now. A lot of that can be done online. And if you decide that a long-term community is a better option, make sure you do your due diligence and find the right place for you and your loved one. I
Theresa Wilbanks, family caregiver, author and advocate
Re-imagine self-care: You may not have recognized your hobbies and interests as self-care before caregiving. Going to the gym, reading for pleasure, spending time with friends was just a part of life.
As we begin to care for a family member and priorities shift, it is not uncommon to give up our interests and hobbies bit by bit until our entire life revolves around caregiving. When possible, it is better to share the caregiving responsibilities by delegating or accepting help so that you can continue to participate in your passions.
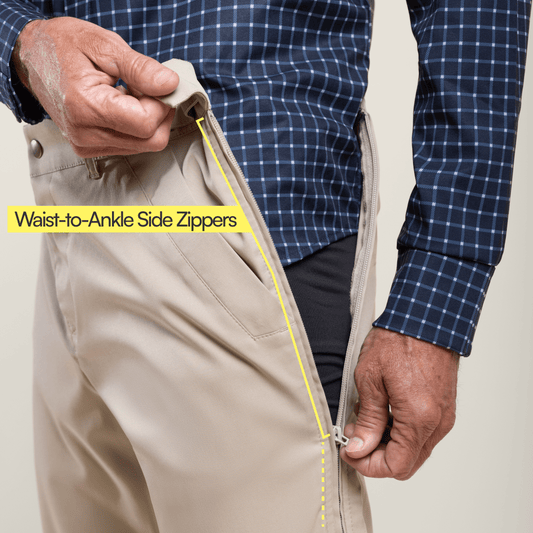
Peter Zollo, cofounder of Joe & Bella and former family caregiver:
There’s an adjustment period. When you make the move – whether it’s the first time into any senior-living community or you’re moving to another community – expect that your loved one will feel out of sorts and will likely take a step back in any behavioral improvement they’ve recently demonstrated. For those with and without cognitive disabilities, moving is never easy – finding your own space in a new place is scary. We all hear about the importance of getting out of your “comfort zone.” I’d say the opposite is true for older adults; you want to find that zone and keep them in it. So, moving older loved ones to a new community will almost always result in older adults taking a step back. When I moved my mom into her third community, I asked the Executive Director about this very issue, as I was concerned that my mom didn’t seem like herself -- that she seemed less social, less confident, less joyful. Jen, the ED, told me to give it eight weeks until she’d be hopefully 100% back. I thought at the time that was a crazily long time to wait. Jen was right.
For more inspiring caregiving advice, check out Dementia Caregiver Tips from the "Dementia Darling" and parts 1 of 2 of "The Reluctant Caregiver" with Joy Johnston.